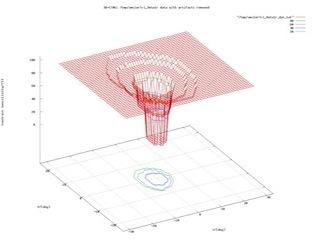
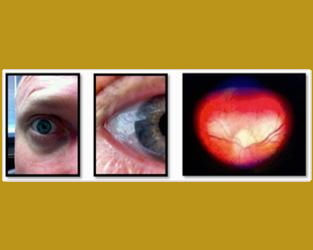
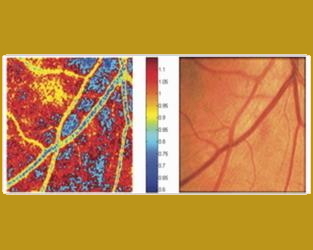
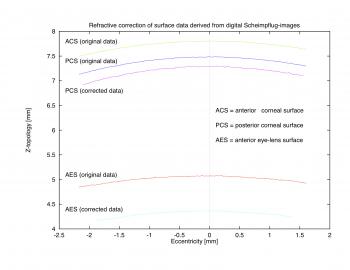
Our purpose is to correct digital CCD-recorded Scheimpflug photographs, imaging both the anterior and posterior corneal surface, the anterior chamber, and the anterior eye lens surface for optical distortions. In a ray-tracing algorithm the imaging of the posterior corneal surface in a given Scheimpflug photograph is corrected by applying Snell's law on parallel incident rays entering through the anterior corneal surface. Once the posterior corneal surface is corrected, the procedure is repeated, again with parallel incident rays entering through both the anterior and now corrected posterior corneal surface, to correct the imaging of the anterior eye lens surface. The refractive indices necessary for Snell's law are taken from Gullstrand's exact schematic eye model. Due to the optical/refractive correction, the digital Scheimpflug photograph decreases in size perpendicular to the direction of the optical axis. As a consequence the curvature radii of both the posterior corneal surface and the anterior lens surface are reduced significantly, as compared to the original digital Scheimpflug photograph. Furthermore, the corneal thickness and the anterior chamber depth are increased. The presented refractive correction method enables us to extract from Scheimpflug photographs the following quantities rather realistically: structure coordinates and curvature radii of both the posterior corneal surface and the anterior lens surface, corneal thickness, and anterior chamber depth. This method can readily be applied to other imaged quantities, such as the posterior eye lens surface, the lens thickness, and the pupillary opening.
Biomedicine
We have developed user-friendly, non-invasive external readout systems to obtain (optically) information from, e.g., the anterior chamber of the eye such as but not limited to indicated intraocular pressure (IOP) from an implanted IOP sensor, fill-level of implanted drug delivery systems, status monitoring of glaucoma relieve valves/shunts, and other physiological conditions. Two designs have been devised and prototyped: (1) an indirect digital camera-based reader, and (2) a direct opto-mechanical reader. The digital reader comprises an off-the-shelf consumer digital camera (5 MP) that has been modified, i.e., equipped with custom adapter and custom lens to shorten the focal length for close-up imaging. Focus is maintained with the built-in autofocus. The opto-mechanical reader is a U-shaped binocular, using only optical components, i.e., lenses and prisms/mirrors to reroute the optical pathway. The user monitors with one eye the anterior chamber of the respective other eye in magnification, and vice versa. The focus of the optical lens system and the width between the two eyepieces of the opto-mechanical reader are user-adjustable. The digital reader images the eye at about 20-50x magnification. For example, it takes a snapshot of the iris, which may carry an implanted sensor (e.g., MEMS-based IOP sensor attached to the iris) and displays the image on the built-in LCD viewer. With the optical zoom engaged the reader currently achieves a resolution of about 5mm per pixel and with the additional digital zoom a resolution of about 1.2mm per pixel. These performance parameters are camera-dependent, i.e., they are linearly coupled to the horizontal and vertical camera resolution at hand. The opto-mechanical reader achieves currently a 20-50x magnification. The digital reader utilizes off-the-shelf consumer digital cameras and hence may provide a low-cost digital microscope capability. The advantage of the opto-mechanical reader is that it does not require any type of camera, image processing, or other electronic parts. Both reader designs may enable users to image or self-examine their eyes without the help of others. They may assist the treatment and management of glaucoma.
[Issued patent(s): U.S. 7,481,534 and U.S. 7,762,664]
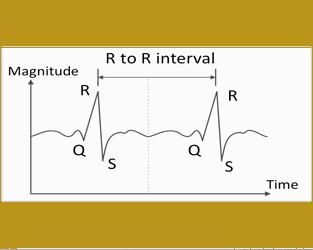
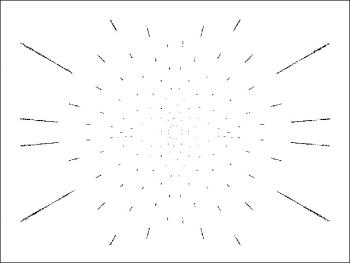
Ray tracing with a computer allows realistic simulation of optical properties of the human eye. Patterns of point sources are used as objects. The path of light rays is calculated between the point source and the retina for a Gullstrand exact schematic eye model with improved parameters; the normal eye model has a resolution limit close to the natural resolution limit of the human eye. The image formed on the retina is projected back to a screen at the distance of the object so as to simulate image interpretation by the brain. Refractive errors are modeled by a change in eye parameters and corrected by eyeglasses or/and contact lenses or by an artificial intraocular lens. For optic correction the parameters of seeing aids can be fitted automatically by a least-squares routine.
Sponsor(s):
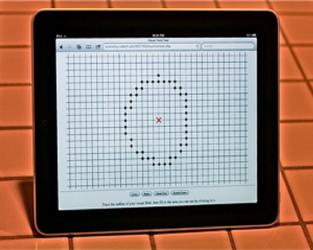
To provide a validated visual field test and analysis system that is worldwide accessible via the Web, to allow for multi-center clinical studies performed on touchscreen-equipped computers and touchpad devices, such as iOS-based handhelds (i.e., iPad, iPhone, iPod).
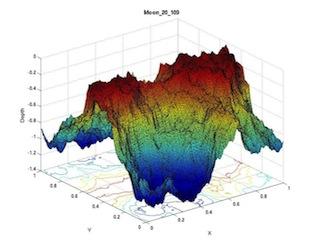
The Web-based visual field test and analysis system employs the 3D Computer-automated Threshold Amsler Grid (3D-CTAG; Fink & Sadun, J Biomed Opt 2004) as its testing method: While positioned on a head-chin rest, patients trace areas on a touchscreen simulating an Amsler grid at varying levels of contrast. This plots the boundaries of areas missing from their field of vision. The result is a 3D data set that represents the (central) visual field and occurring scotomas within at each contrast level.
A centralized, Webserver-based integrated visual field test and analysis system allows for multi-center clinical studies. Furnished with a Web-portal, administrative access is provided to physicians to manage their respective patients, and subsequent patient access is granted to undergo testing with 3D-CTAG. Following each visual field test, the patient-ID-tagged but otherwise anonymous examination data are transmitted to the server for database storage and processing. Several graphical depictions of the visual field (i.e., hill-of-vision) and objective visual field analysis data (i.e., characterization indices; You & Fink, ARVO 2010) are generated on the server and subsequently displayed on the computer or touchpad device where the test was administered (i.e., client). Both the patient and the assigned physician can access the stored patient data at a later time to regenerate the graphical output and analysis data on demand. The visual field test and analysis system can be hosted both locally (i.e., standalone) and centrally (i.e., server-based global access), and is accessible to touchpad devices affording mobility and deployment in the field.
The validated visual field test and analysis system enables worldwide subject screening and examination via the Web, provides an objective analysis of visual fields and scotomas within, and offers a promising perspective towards modern computer-assisted diagnosis in both medicine and telemedicine. As opposed to conventional visual field tests, 3D-CTAG, which is at the core of the Web-based system, is capable of monitoring central visual field loss due to macular degeneration. Its clinically demonstrated capability of early detection of glaucoma and macular degeneration allows for timely countermeasures to help prevent irreversible blindness. As such it may have the potential to change the standard of visual field examinations.
[Issued patent(s): U.S. 6,578,966, E.P. 1,276,411, U.S. 6,769,770, and U.S. 7,101,044]
Sponsor(s):
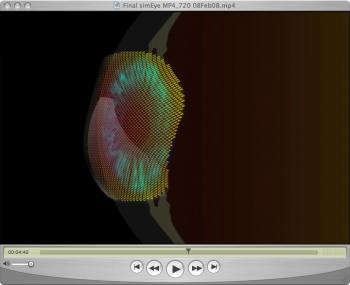
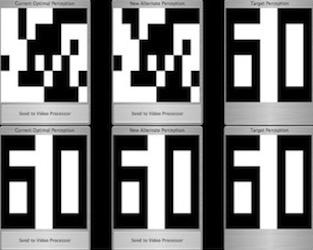
The computer ray tracing tool developed here (SIMEYE) permits simulations of the optical properties of the human eye and of visual perception under various eye defects, both as still-images and as animated movies. SIMEYE allows for the introduction of arbitrary surfaces (e.g., aspheric surfaces), represented/fitted by a set of Zernike polynomials, in the ray tracing simulation. SIMEYE may have a wide range of applications in both science and education. This tool may help educate/train both the lay public, e.g., patients before undergoing eye surgery, and people in the medical field such as medical students and professionals. Moreover, SIMEYE may be used as a scientific research tool to investigate the visual perception under a variety of eye conditions, in addition to the ones presented here, and after various ophthalmic surgical procedures such as cataract surgery and LASIK.
Sponsor(s):
Adequate correction is an essential prerequisite for precise perimetry. Therefore, not only the correct glasses have to be chosen, but also their positioning should be properly determined. Otherwise, a distortion of the stimulus grid, as well as a (area enlarging/reducing) distortion of the stimuli themselves, can occur. Therefore, scotomata may be simulated in visual fields which are purely optically evoked (so-called refraction scotomata), because the light stimulus is mapped on an enlarged/reduced retinal area, thereby reducing/increasing light density.
Derived from models of neural networks, a model for the pupillary pathway is introduced that can easily be handled computationally and analytically. To model the binocular pupillary reactions we use a feed-forward network, namely, a multi-layered perception. It is possible to calculate the pupillary reactions analytically as a function of the light stimuli of the retinal hemifields, on the one hand, and the set of neural couplings between the neural layers, on the other. Several lesions, e.g., lesions of the intercalated neurons between the afferent and efferent pupillary pathways, can be simulated within the model and the corresponding pupillary reactions such as anisocoria or relative afferent pupillary defects (RAPD) can be calculated analytically. Due to its neural network structure the model described herein can easily be extended to much more complex pupillary pathways while remaining calculable computationally and analytically.
The simulation environment, the project Eyemovie was created in, offers an objective way to actually see how various eye defects affect the visual perception of a patient. It is incomparably more instructive than having the patient describe and explain what he perceives. Aside from being an ideal educational tool the simulation environment represents a highly versatile scientific investigational tool to simulate before and after scenarios as they occur in, e. g., cataract and refractive laser surgery. Given a more advanced eye model adjustable to individually measured biometric and topographic real eye data, much more realistic simulations may be performed: effects of refractive laser surgery techniques, tear film distortions (dry eyes), multi-focal IOLs, etc.
Sponsor(s):
An Internet-based classification system for visual field data, like the one proposed here, furnishes a valuable first overview in judging perimetric examination results and gives an indication towards the final diagnosis by a physician. It should not be considered a substitute for the diagnosing physician. However, thanks to the world-wide accessibility of the Internet the classification system offers a promising perspective towards modern computer-assisted diagnosis in medicine.

We have been developing implantable intraocular pressure sensor devices for detecting excessive intraocular pressure above a predetermined threshold pressure to assist Glaucoma therapy. These devices include MEMS pressure switches that are sized and configured to be placed in an eye, wherein said pressure switch is activated when the intraocular pressure is higher than the predetermined threshold pressure. The intraocular pressure sensor devices are optically powered and transmit data wirelessly using optical communication.
[Issued patent(s): U.S. 7,131,945, U.S. 7,481,534, and U.S. 7,762,664]